U.S. Healthcare Payer and Employer Market Size, Share, and COVID-19 Impact Analysis, By Service Offering (Medical Coverage, Dental Coverage, Vision Coverage, and Others), By End-User (Public Payers, Private Payers, and Employer Groups), and US Healthcare Payer and Employer Market Insights, Industry Trend, Forecasts to 2035
Industry: HealthcareUnited States Healthcare Payer and Employer Market Insights Forecasts to 2035
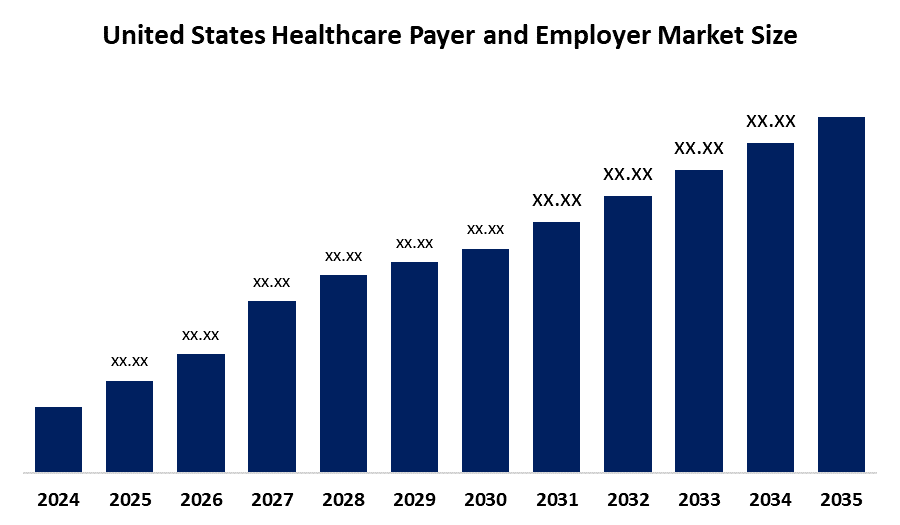
- The US Healthcare Payer and Employer Market Size is Expected to Grow at a CAGR of around 7.3 % from 2024 to 2035
- The U.S. Healthcare Payer and Employer Market Size is Expected to Reach a significant share by 2035.
Get more details on this report -
According to a research report published by Spherical Insights & Consulting, The United States Healthcare Payer and Employer Market Size is Expected to Grow 7.3% CAGR from 2024 to 2035, is Expected to Reach a Significant share by 2035. Driven by the expansion of Medicaid coverage across states, the growing adoption of value-based care models, and the growing demand for digital health technologies. Furthermore, payers are being prompted to innovate and streamline their operations by regulatory reforms such as the No Surprises Act and the increased emphasis on social determinants of health.
Market Overview
In the U.S. healthcare system, a payer refers to any organization that finances or reimburses the cost of medical services is referred to as a player in the U.S. healthcare system. This covers commercial insurance providers, self-funded employer plans, and government programs like Medicare and Medicaid. Payers process claims, oversee insurance coverage, and bargain with providers over prices. In this sense, an employer is a business or organization that offers health insurance to its workers, either by directly paying for medical expenses through self-insured arrangements or by purchasing group plans from insurers. Employers are crucial to coverage access, particularly for people of working age. Additionally, the growing demand for digital health solutions, the growing adoption of value-based care models, and rising healthcare costs all present strong growth prospects for the US healthcare payer and employer market. Employers are increasingly moving toward self-funded health plans in order to obtain flexibility and control over benefit design, while payers are investing in advanced analytics, artificial intelligence platforms, and outsourced services in order to manage claims, enhance member engagement, and control costs. The market is also witnessing an increased demand for consumer-directed health platforms, third-party administrators, and specialty benefit management due to the combined $4 trillion in government and commercial healthcare spending.
Report Coverage
This research report categorizes the market for the United States healthcare payer and employer market based on various segments and regions and forecasts revenue growth and analyses trends in each submarket. The report analyses the key growth drivers, opportunities, and challenges influencing the US healthcare payer and employer market. Recent market developments and competitive strategies such as expansion, product launch, and development, partnership, merger, and acquisition have been included to draw the competitive landscape in the market. The report strategically identifies and profiles the key market players and analyses their core competencies in each sub-segment of the U.S. healthcare payer and employer market.
United States Healthcare Payer and Employer Market Report Coverage
| Report Coverage | Details |
|---|---|
| Base Year: | 2024 |
| Forecast Period: | 2025-2035 |
| Forecast Period CAGR 2025-2035 : | 7.3% |
| Historical Data for: | 2020-2023 |
| No. of Pages: | 225 |
| Tables, Charts & Figures: | 119 |
| Segments covered: | By Service Type, By End-User |
| Companies covered:: | UnitedHealth Group, Kaiser Permanente, Centene Corporation, Humana Inc., Molina Healthcare, and Others |
| Pitfalls & Challenges: | COVID-19 Empact, Challenges, Future, Growth, & Analysis |
Get more details on this report -
Driving Factors
Increasing medical expenses, aging populations, and the prevalence of chronic diseases are the main factors influencing the U.S. healthcare payer and employer market. To cut costs, employers are switching to self-funded plans, and payers are spending money on value-based care, analytics, and digital platforms. Specialty benefit management, transparency requirements, and regulatory changes all hasten innovation and market development.
Restraining Factors
Rising medical inflation, a lack of clarity in regulations, shrinking profit margins, and a lack of workers are some of the factors that are limiting the U.S. healthcare payer and employer market. Scalability is further hampered by complicated reimbursement schemes, narrow rate flexibility, and heavy administrative costs, and competition and innovation among payer networks are diminished by consolidation.
Market Segmentation
The United States healthcare payer and employer market share is classified into service offering and end-user
- The medical coverage segment held a significant share in 2024 and is expected to grow at a significant CAGR during the forecast period.
The US healthcare payer and employer market is segmented by service offering into medical coverage, dental coverage, vision coverage, and others. Among these, the medical coverage segment held a significant share in 2024 and is expected to grow at a significant CAGR during the forecast period. The segmental growth is driven by its widespread use in both the public and private sectors, as well as its crucial role in employer-sponsored plans. Following as supplemental benefits, dental and vision coverage are becoming more popular as a result of increased awareness of preventive care and employee wellness initiatives. Other services make a minor contribution to the market's overall growth.
- The private payers segment held a significant share in 2024 and is expected to grow at a significant CAGR during the forecast period.
The US healthcare payer and employer market is segmented by end-user into public payers, private payers, and employer groups. Among these, the private payers segment held a significant share in 2024 and is expected to grow at a significant CAGR during the forecast period. Driven by the prevalence of employer-sponsored health plans and commercial insurance companies. More than 65 percent of Americans have private insurance, and this market leads in terms of digital innovation, benefit customization, and claims volume. Employer and public payer organizations then follow suit, adding to cost-control and coverage diversity initiatives.
Competitive Analysis:
The report offers the appropriate analysis of the key organizations/companies involved within the U.S. healthcare payer and employer market along with a comparative evaluation primarily based on their product offering, business overviews, geographic presence, enterprise strategies, segment market share, and SWOT analysis. The report also provides an elaborative analysis focusing on the current news and developments of the companies, which includes product development, innovations, joint ventures, partnerships, mergers & acquisitions, strategic alliances, and others. This allows for the evaluation of the overall competition within the market.
List of Key Companies
- UnitedHealth Group
- Kaiser Permanente
- Centene Corporation
- Humana Inc.
- Molina Healthcare
- Others
Recent Developments:
- In February 2023, CVS Health had entered into a definitive agreement to acquire Oak Street Health in an all-cash transaction for $39 per share, representing an enterprise value of approximately $10.6 billion. The company had financed the transaction with borrowings of $5.0 billion from a term loan agreement executed on May 1, 2023, along with existing cash and available resources. CVS Health had remained committed to maintaining its credit ratings.
Key Target Audience
- Market Players
- Investors
- End-users
- Government Authorities
- Consulting and Research Firm
- Venture capitalists
- Value-Added Resellers (VARs)
Market Segment
This study forecasts revenue at US, regional, and country levels from 2020 to 2035. Spherical Insights has segmented the United States Healthcare Payer and Employer Market based on the below-mentioned segments:
United States Healthcare Payer and Employer Market, By Service Type
- BPO Services
- ITO Services
- KPO Services
United States Healthcare Payer and Employer Market, By End-User
- Public Payers
- Private Payers
- Employer Groups
Need help to buy this report?